Primary primitive neuroectodermal tumor of the cervix confirmed with molecular analysis in a pregnant woman: A case report and literature review
Introduction
Primary primitive neuroectodermal tumor (PNET) is a highly malignant tumor characterized by neuroectodermal and neural crest cells’ origin, most of which arise from the central nervous system, soft tissues, and bones (Rajwanshi et al., 2009). In more than 90% of PNET cases, chromosomal translocations result in the fusion between the EWS gene (also known as EWSR1, Ewing sarcoma breakpoint region 1) and a member of the ETS family of transcription factors, such as FLI1 and ERG (Song et al., 2012).In this article, we presented a case of cervical PNET diagnosed during pregnancy whose tumor grew very rapidly. The patient terminated her pregnancy, and was treated with surgical resection, adjuvant chemotherapy, followed by pelvic radiotherapy. To gain a deeper understanding of this rare disease, we reviewed PNET-related literature and found 26 cases of primary cervical PNET, including 5 cases occurring during pregnancy.
Case report
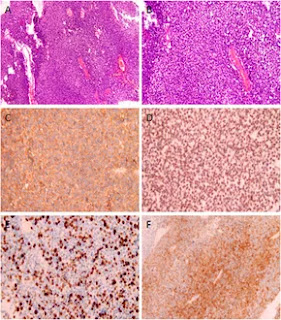
A 29-year-old female, gravida 1 para 0, was referred to her obstetrician at the 7th week of gestation. An ultrasonography examination revealed a cystic-solid mass measuring 5 cm × 4 cm in the cervix. Her medical and family history were not significant. No additional examinations or treatments were performed because of her pregnancy. During follow-up, the ultrasonography examination demonstrated that the mass grew rapidly, and at the 20th week, the patient was admitted to our department because she began to complain of low back pain. An MRI was performed and it was found that the mass grew to 11 cm × 10 cm × 10 cm in just 2 months. The levels of CA-125, CEA, SCC, and NSE were normal. Considering the pregnancy, the patient refused biopsy and chose to continue observation.However, at the 22nd week of gestation, the patient was referred to the emergency department because of vaginal watery discharge. Gynecological examination showed that there was a rupture on the surface of the tumor and fluid was flowing out of the rupture, which was thicker than amniotic fluid. The result of amniotic fluid crystallization was negative. In addition, MRI showed the cystic-solid mass was smaller (10 cm × 8 cm × 7 cm) than before. Bimanual pelvic examination revealed the tumor was in the cervix, without invading the vagina, or adjacent organs (Figure 1). The patient underwent a biopsy of the cervical mass, and it was found that the tumor consisted of small round cells and had extensive necrosis. IHC showed that tumor cells expressed CD99, synaptophysin (SYN), friend leukemia integration 1 (FLI1), and P16. However, no expression of cytokeratin (CAM5.2), P53, chromogranin A (CgA), CD56, or neuron specific enolase (NSE) was detected. Ki-67 proliferation index was about 80% (Figure 2). A pathological diagnosis of cervical PNET was suspected. Next, we performed FISH to detect the presence of the chromosomal translocation t (11;22, q24;q12). A section of 4 μm was cut from paraffin-embedded biopsy blocks and stained with hematoxylin-eosin in order to confirm the presence of tumor cells and to choose the appropriate area for the hybridization procedures. A specific translocation separation probe kit (Vysis, United States ) was used, which consisted of two probes; one directly labeled with red fluorescence and bound to 3′ end of the FLI1 (11q24) gene, and the second directly labeled with green fluorescence and bound to 5′ end of the EWSR1 (22q12) gene. According to the manufacturer’s instructions, 200 nuclei with fluorescence signal were randomly selected to observe the number of nuclei with hybridization signal by using a Zeiss Axioplan fluorescence microscope (Zeiss, Germany). Nuclei with the EWS-FLI1 fusion gene showed yellow signals, while nuclei without gene translocation showed separate red and green signal. The criterion for a positive result of the EWS-FLI1 fusion gene was that more than 10% of the nuclei showed a fusion signal. FISH demonstrated that more than 35% of the cells were positive, indicating the presence of the EWS-FLI1 fusion gene (Figure 3A). In order to clarify the type of fusion, we performed RT-PCR test. Total RNA was isolated using TRIzol (Gibico, United States ) and the concentrations were measured by NanoDrop-2000c (Thermo Fisher Scientific, United States ). Transcriptor high fidelity cDNA synthesis kit (Takara, Japan) was used for reverse transcription of 1 μg of RNA from the sample. RT-PCR was carried out using SYBR Green Master Mix (Roche, Switzerland) in a Quantstudio3 real-time thermal cycler (Thermo Fisher Scientific, United States ). Expression data were normalized to GAPDH. The primer sequences used for RT-PCR analysis of EWS-FLI1 were as follows; 5′- CCAAGTCAATATAGCCAACAG-3′ and 5′-GGCCAGAATTCATGTTATTGC-3’. RT-PCR products were analyzed on a 2% agarose gel electrophoresis. The results showed the RT-PCR product of the tumor was 166bp, which indicated that the 7th exon of EWS was fused to the 5th exon of FLI1 (Figures 3B,C). These results confirmed the diagnosis of cervical PNET.
Conclusion
PNET in the female reproductive tract is an extremely rare disease. In this article, we reported a case of cervical PNET complicated by pregnancy. The diagnosis of PNET depends on pathology, immunohistochemistry, and genetic analysis. Molecular analysis may significantly contribute to the final diagnosis of PNET occurring in this unusual location. In addition, the type of EWS-FLI1 fusion may be related to clinical outcomes. At present, the effective treatment for PNET is surgery combined with chemotherapy and radiotherapy. The rapid growth of PNET during pregnancy may be related to hormonal changes and further research is needed.Follow on:
Facebook https://www.facebook.com/
Twitter https://twitter.com/home?
Blogger https://www.blogger.com/u/1/
Youtube https://www.youtube.
Pinterest https://in.pinterest.com/
Linkedin https://www.linkedin.com/
Instagram https://www.
Blogger https://www.blogger.com/u/1/
Youtube https://www.youtube.
Pinterest https://in.pinterest.com/
Linkedin https://www.linkedin.com/
Instagram https://www.





Comments
Post a Comment